Inflammation
Pain is the leading cause of physical and psychological suffering in the UK, with up to 50% of the population experiencing ongoing chronic persistent pain. With the ageing population, this figure is set to rise even further in the coming years. Importantly, many people have multiple sources of pain, including muscle and nerve pain, and conventional treatments may often be of only limited help.
Living with chronic persistent pain has a tremendous impact on psychological and physical wellbeing with many patients experiencing sleep disturbances, disruptions in social relationships, decreased cognitive function, decreased physical functioning, interference with activities of daily living, decreased productivity, increased anxiety and depression, and decreased quality of life.
Some of the most common conditions associated with chronic pain are:
• Back pain
• Osteoarthritis
• Headaches and migraine
• Inflammatory bowel disorder
• Musculoskeletal injury and trauma
• Rheumatoid arthritis
• Fibromyalgia and chronic fatigue syndrome
• Autoimmune disease
The inflammatory process
Common to all of these conditions is inflammation (from the Latin inflammatio, to set on fire). Inflammation is a complex biological response by the body to injury or assault, as it attempts to remove the stimulus and initiate tissue healing. It manifests as symptoms such as swelling, heat and redness with attendant pain as blood flow increases to the affected area and immune cells accumulate to eliminate the cause of injury and initiate the healing process.
Although inflammation is a normal part of the healing process, when it becomes prolonged and if left untreated, it can cause numerous problems. Chronic inflammation can result when the body’s immune system is “tricked” into attacking its own soft tissue as though it was an invader, resulting in tissue destruction and the development of a host of chronic conditions.
Pain killers aren’t the only solution
Current strategies for pain management rely largely on medications. Unfortunately, as society’s need for pain management increases, so does awareness about the risks of pain relieving drugs. Increasing evidence of serious health risks, including organ damage and death, have left patients and health professionals looking for safer alternatives. In addition, traditional painkillers are rarely effective at reducing nerve pain.
A new approach to pain relief
Fortunately, recent advances in nutritional science have led to the development of highly effective natural approaches to pain management. By combining safe and effective lifestyle and nutritional strategies, the underlying causes and mediators of chronic persistent pain can be successfully addressed, providing long-lasting relief from pain, invariably leading to vast improvements in psychological and physical wellbeing.
Controlling inflammation through diet
What we eat contributes significantly to how we feel. Fresh, whole organic foods can contribute to good digestion and metabolism, and many of these foods are considered “anti-inflammatory”. Other foods can be “pro-inflammatory” causing pain and inflammation to increase. Some foods, specifically plants from the nightshade family (eg tomatoes, peppers, aubergines & white potatoes) contain a compound called solanine, which can cause inflammation in certain individuals and should therefore be avoided.
If you suffer from chronic persistent pain, it may be helpful to follow these dietary guidelines:
Healthy foods to include:
Brown rice • oats • quinoa • beans • lentils • chicken • turkey • lamb • oily fish • green leafy vegetables • broccoli • carrots • parsnips • nuts (not peanuts) • seeds • non-citrus fruit • spices • and plenty of water.
Foods to avoid:
Wheat/gluten • dairy products • eggs • red meat • processed meats • shellfish • peanuts • citrus fruits • white potatoes • tomatoes • peppers • aubergine • sugar • sweeteners • fizzy/sugary soft drinks • coffee • tea • and alcohol.
Helpful herbs and nutrients
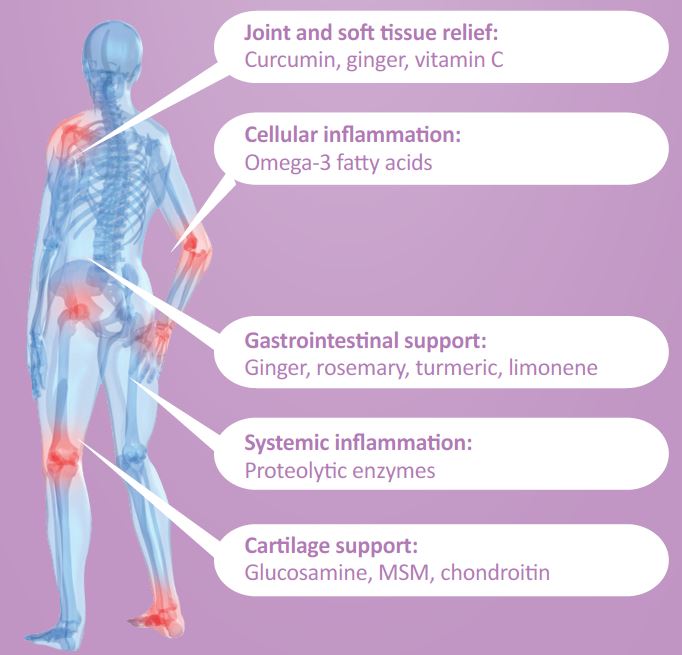
Numerous nutrients, botanicals and enzymes have been shown to help with pain, inflammation and soft tissue health.
In addition to making dietary modifications as described above, it may also be helpful to supplement with nutritional formulas containing natural substances from foods, plants and herbs that have been shown to act as natural, safe inhibitors of pain and inflammation.
Essential Fatty Acids
In particular omega-3 fatty acids from fresh oily fish, are converted into potent anti-inflammatory substances in the body.
Herbs &; Spices
Numerous culinary herbs and spices have been shown to have excellent antioxidant and anti-inflammatory properties, thereby helping to reduce inflammation and swelling. These include:
• Turmeric / Curcumin
• Ginger
• Cayenne
• Rosemary
Antioxidants and bioflavonoids
Naturally-occurring components of fruits and vegetables, antioxidants and bioflavonoids have been shown to reduce the release of inflammatory mediators. Such compounds include:
• Vitamin C
• Quercetin
• Rutin
• Limonene
Proteolytic enzymes
Proteolytic enzymes, such as bromelain, papain, pancreatin, trypsin, chymotrypsin and serrapeptase have been shown to act as regulators and modulators of the inflammatory response.
This information is reproduced from Nutri Advanced here https://www.nutriadvanced.co.uk/library/educational-literature/information-guides/inflammation-the-facts.html?utm_source=Healthcare+Professional+Newsletter&utm_campaign=16da85cad7-ECRM251&utm_medium=email&utm_term=0_b9139ffb25-16da85cad7-354479313&mc_cid=16da85cad7&mc_eid=3061371ebf
For more information on our expert formulations or any other products, please ask during your treatment for guidance on how to order.